Mental and Physical Health Parity
|
Mental Illness Still Isn't Treated the Same as Physical Illness, Especially in Children
|
With the passage of the Affordable Care Act in 2010, mental healthcare was given what’s called “parity” with physical healthcare. This meant that insurance companies could no longer refuse to cover mental health treatment, nor could plans impose higher cost-sharing models on mental healthcare than on physical healthcare.
|
At the time, this was heralded as an enormous step forward in the effort to destigmatize mental illness and to increase access to treatment.
Sadly, this new era of acceptance and improved access hasn’t materialized. Nowhere is this more evident than in the struggle to access mental healthcare for children, and in the lack of support offered to their families.
|
What Happens With Physical Illness
|
When a child is diagnosed with a chronic physical illness such as juvenile diabetes, their medical providers, and often the hospital systems in which they practice, work to make sure the parents have the resources they need to effectively support their children. Parents are provided counseling on nutrition and medications, support and encouragement from nursing staff, educational classes for how to manage the disease on a day to day basis, and opportunities to meet other parents and families on the same medical journey. Families receive reading material, access to online resources, a 24-hour nursing line, and myriad age appropriate kits and tools for the child to help them acclimate to living with this new diagnosis.
|
In short order, families become experts on the signs and symptoms of high and/or low blood sugar, how to properly administer insulin, and what accommodations the child needs to be safe and thrive across various settings, from school to soccer practice. Parents want to learn all they can in order to meet their child’s needs, see their child thrive, share the best possible quality of life,
|
and achieve stability and wellness. They are given the tools to make that possible.
|
What Happens With Mental Illness
|
Let’s contrast this example with what happens when a child is diagnosed with a mental health disorder like bipolar. When the child’s diagnosis is a mental illness, these kinds of comprehensive support systems not only aren’t offered, they are, quite simply, unavailable in most places. Families are left feeling confused, with little context for understanding the diagnosis or the medication that may be prescribed. Families are unsure where to go to get the information and resources they need, they are embarrassed by the stigma still attached to mental illness, they feel isolated, and they don’t have the guidance and tools they need to best help their children.
|
So how do we create equity between mental health and physical health? For starters we have to remember that living with a mental illness is the same thing as living with a medical condition.
|
In both cases, families need a comprehensive support system in order to understand and navigate the challenges posed by their child’s illness, and in order to achieve long term stability and disease management. Whether the diagnosis is diabetes or bipolar disorder, they must be able to learn as much as they can, and have access to as many resources as possible, delivered by a diverse and supportive community of providers and peers.
If we take the example of a child living with bipolar, it is vital that parents be able to recognize the symptoms of depression, mania, mixed mood episodes, and ultra rapid cycling. These episodes must be identified and understood as symptoms, and differentiated from willful behaviors so the symptoms can be treated appropriately by family, teachers, and caregivers. Symptoms, triggers, and coping skills’ developments also need to be reported accurately to providers, in order to inform treatment decisions.
|
How Kids Benefit From Treatment
|
Children and adolescents benefit most from treatment when their caregivers are able to partner with providers. With effective communication, caregivers and providers can together make decisions about medications, therapeutic interventions, and lifestyle changes that will best support symptom management. This requires that parents know and understand terminology, what symptoms look like, how to identify when they are present, which medications are effective in treating their child’s illness and which are contraindicated, what symptoms each medication is targeting, and how to assess the impact those medications have.
Parents also need to be educated on how to identify when they’re experiencing a mental health emergency and what to do during it. Families must know how to de-escalate a crisis, how to keep track of presenting symptoms and triggers, who to contact for help, when to call 911, and what information to give emergency responders. It is not reasonable to expect that parents and caregivers should understand how to do all of these things without guidance, education, coaching, and encouragement.
|
Positive short and long term outcomes come from having a comprehensive and effective treatment plan, as early as possible. If we can provide the same kind of support systems to those with pediatric mental health conditions as are offered to those with pediatric physical health conditions, parenting approaches can be adapted to ease symptoms, decrease triggers, promote
|
wellbeing for everyone in the home, and empower parents to be effective participants in their child’s care.
Currently it is still up to parents to create their own mental health support system, seek out educational materials, and cobble together the resources needed. My colleagues and I at the Children’s Mental Health Resource Center (CMHRC) do what we can to meet these needs through our outreach, advocacy, education, and support. However, truly transformational reform will only come about when we universally and unequivocally accept that mental health IS physical health and that those living with mental illness, must be treated equitably.
|
Elizabeth Errico is a parent, a licensed mental health counselor, and the executive director of the Children’s Mental Health Resource Center.
|
Everything we do at CMHRC, from support for families, to education for providers, to our free resources and events is focused on reaching parity, promoting mental health equity, and reducing stigma.
Our Members make this possible. Make a gift today to support our work and be a part of the solution.
|
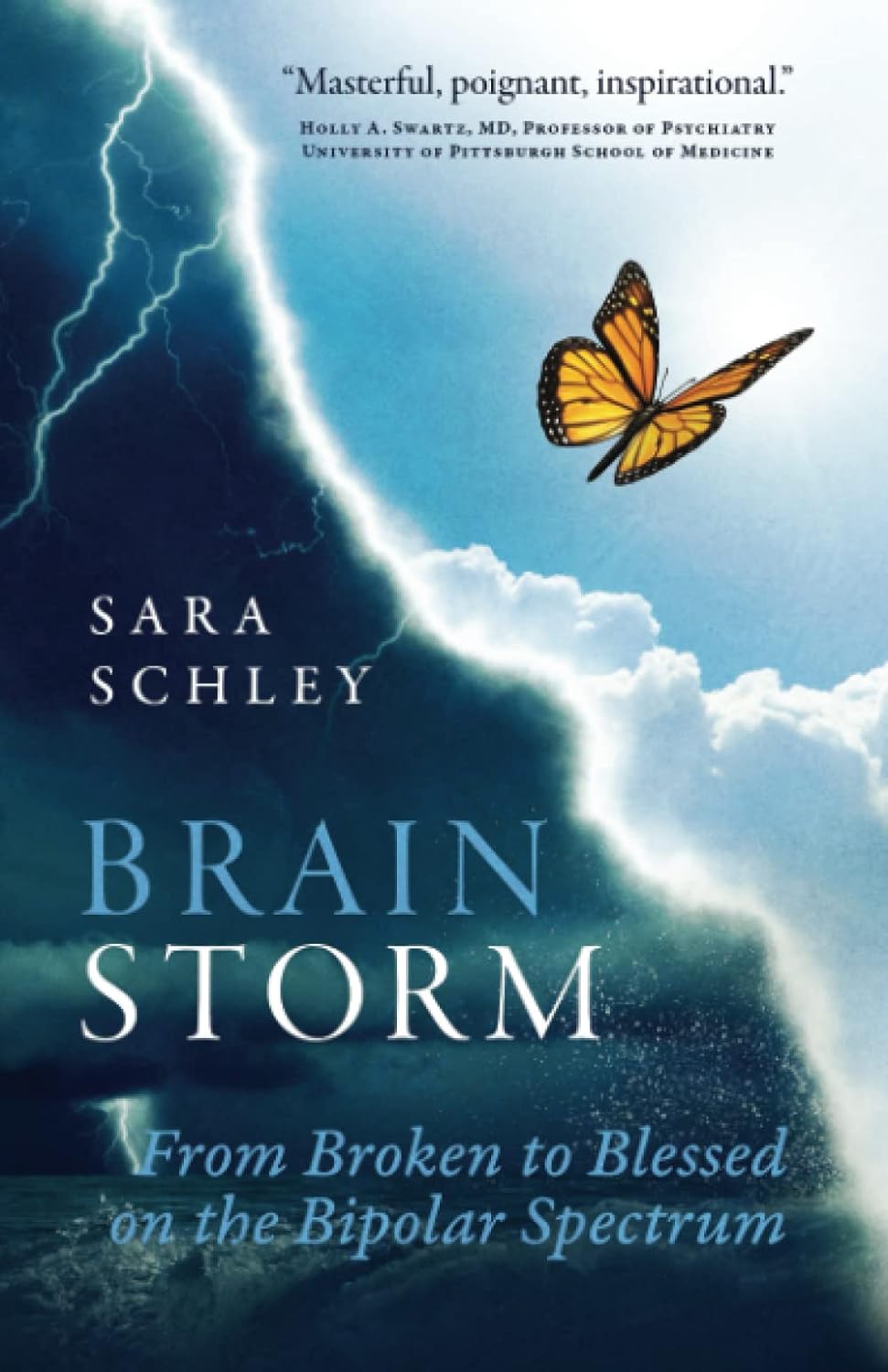
BrainStorm: From Broken to Blessed on the Bipolar Spectrum
Thursday April 18th, 7:30pm Eastern Time
|
You absolutely don't want to miss out on this month's Book Club. Author Sara Schley will be live and in person with our Book Club to discuss her book. Attendees will be invited to ask questions, share their own stories, and dive in with her for an inside look.
In this acclaimed memoir Sara tells her life-changing story to help end the bipolar stigma, optimize brain health, and save lives.
|
ALSO JOIN SARA FOR A WEDNESDAY WEBINAR
|
Bipolar Success with Sara Schley
April 17th, 7:30pm Eastern Time
|
At twenty-one, as a senior in college, Sara was a scholar-athlete who seemed to have it all. Then, like the flip of a switch, she had her first brain breakdown: A tailspin into a living hell. It was terrifying.
It took her twenty-five years and five psychiatrists to get the diagnosis that saved her life: Sara is on the bipolar spectrum with a bipolar II brain. With the correct diagnosis, medication, support, and self-care, people who have experienced severe, persistent depression-which is actually a form of bipolar-can live rich, full lives.
Sara's life is proof.
The self-care disciplines Sara has honed over forty years of living with her bipolar II brain can help anyone who experiences anxiety, stress, or depression heal. Read this book to transform your life or that of someone you love.
|
FREE CLINICAL SEMINAR FOR PROFESSIONALS
|
Differentiating Bipolar & ADHD
April 24th, 5:00pm Eastern Time
|
One of the most common misdiagnoses for kids with bipolar disorder is to be diagnosed with ADHD. Join us for this deep dive into the differences between bipolar disorder and ADHD in terms of symptoms like hyperactivity, impulsivity, and aggression
|
and how they present in each. The presentation will include analysis and discussion of the diagnostic criteria, the role the DSM plays, and will share information from the works of Dr. Charles Popper and Dr. Demitri Papolos (author of The Bipolar Child).
|
|